Connect With Us

Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
What Is Diabetic Limb Salvage?
 Diabetic limb salvage is a medical procedure designed to save the limbs of diabetes patients who have severe foot and leg complications. These limb issues could be infections, ulcers, or tissue damage that are severe enough to lead to amputation. Diabetes can cause poor blood circulation and nerve damage, making it hard for wounds to heal and increasing the risk of infection. The goal of diabetic limb salvage is to treat these conditions effectively, prevent the progression of damage, and maintain as much function of the foot and leg as possible. Various treatments are used, including surgery to improve blood flow, removing infected or dead tissue, and reconstructing the foot if necessary. Diabetic limb salvage is a team effort that includes podiatrists and other specialists working together to create a personalized treatment plan. This approach can not only help save the limb but also significantly improve the patient's quality of life and independence. It is suggested that you add a podiatrist to your care team if you are a diabetic patient experiencing wound healing issues.
Diabetic limb salvage is a medical procedure designed to save the limbs of diabetes patients who have severe foot and leg complications. These limb issues could be infections, ulcers, or tissue damage that are severe enough to lead to amputation. Diabetes can cause poor blood circulation and nerve damage, making it hard for wounds to heal and increasing the risk of infection. The goal of diabetic limb salvage is to treat these conditions effectively, prevent the progression of damage, and maintain as much function of the foot and leg as possible. Various treatments are used, including surgery to improve blood flow, removing infected or dead tissue, and reconstructing the foot if necessary. Diabetic limb salvage is a team effort that includes podiatrists and other specialists working together to create a personalized treatment plan. This approach can not only help save the limb but also significantly improve the patient's quality of life and independence. It is suggested that you add a podiatrist to your care team if you are a diabetic patient experiencing wound healing issues.
Limb salvage can be an effective way in preventing the need for limb amputation. If you have diabetes, cancer, or any other condition that could lead to foot amputation if left unchecked, consult with Andrew Katz, DPM from Allcare Foothealth Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Limb Salvage?
Limb salvage is the attempt of saving a limb, such as the foot from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Diabetes is the number one cause of non-traumatic amputations in the United States. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
However, there are other causes as well, such as cancer and traumatic injury. Links between higher mortality rates and amputation have been found. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our office located in Palmdale, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes, peripheral vascular disease, neuropathy, cancer, and severe crush injury. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If the bone is removed, it is then replaced with prostheses, synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
The Benefits of Everyday Steps

Regular walking, with many people aiming for 10,000 steps a day, is beneficial for foot health, joint function, and overall mobility. Walking strengthens foot and ankle muscles, improves circulation, and enhances joint flexibility, reducing the risk of foot problems and arthritis. It also helps maintain a healthy weight, alleviating pressure on the feet, and preventing conditions like plantar fasciitis. Podiatrists play a vital role in guiding individuals toward safe walking routines. They assess foot biomechanics, recommend suitable footwear, and provide tailored exercise plans. Additionally, podiatrists detect early signs of foot issues and intervene promptly, ensuring optimal foot health. Incorporating regular walking, under a podiatrist's guidance, promotes healthy feet, joints, and overall mobility, whether reaching for 10,000 steps or simply embracing a more active lifestyle. If you want healthier feet and joints through a regular walking routine, it is suggested that you schedule an appointment with a podiatrist for guidance.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact Andrew Katz, DPM from Allcare Foothealth Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctor to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our office located in Palmdale, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Exercise for Your Feet
Foot and ankle pain can be a nuisance in a person’s life, especially if it happens frequently. The best way to prevent this type of pain, is to exercise often. Regular exercise of the foot includes stretching and strength exercises. Stretching exercises can help prevent injuries such as a sprained ankle, while strength exercises can prevent ailments such as plantar fasciitis.
Stretching exercises can help improve flexibility and the foot and ankle’s range of motion. These exercises can certainly help with those who participate in high-energy activities such as sports. Many athletes routinely perform foot and ankle exercises to prevent injuries like sprained ankles, which are common injuries where the tendons in the ankle are over stretched. Strength exercises help develop foot muscles for better support and protection.
Most exercises are simple and can be done at home, either standing or sitting. One chair exercise is called “limber up”. In this exercise, a person would start by sitting down with their feet flat on the floor. Then lift one leg up so the feet are not touching the floor, then rotate your foot clockwise 15-20 times, and 15-20 times counterclockwise. Repeat the same process with the opposite leg. Another sitting exercise helps stretch the back of your heel and requires an exercise band. It begins by looping the band around a heavy piece of furniture, or something stable that will not be moved when the band is tugged or pulled. Then sit directly in front of it, and slide one foot into the loop, so that the band curves around the forefoot. Start by pulling the forefoot back and holding it for 5-10 seconds. Doing this 10-15 times on each foot, will stretch the back of your heel, increasing your flexibility.
Foot exercises that require standing are also just as easy and simple. Referred as the “Achilles Stretch”, this exercise stretches the Achilles tendon, making it more flexible, helping prevent foot, ankle, and leg pain. It begins by first standing and facing the wall, with the arms outstretched and the palms on the wall. Then place one foot behind another keeping the back leg straight, and the forward leg bending at the knee. Make sure both heels are flat on the floor and adjust your stance accordingly. With your hips, lean forward to feel the stretch, you can also adjust the distance from your feet to feel the stretch in various parts of the calf. Make sure to hold the stretch for about 30 seconds and repeat the same process 3 times with each leg. An even easier foot exercise is simply walking on sand. Walking barefoot on sand both strengthens and stretches your feet.
Doing these exercises regularly can help prevent many foot and ankle problems. Other foot exercises can even relieve pain. For example, those affected with plantar fasciitis can simply sit down on a chair, and then place a tennis ball below their affected foot. By rolling the ball under the foot, and increasing or decreasing pressure, pain will be relieved. With any exercise, it is always important to do a small warmup such as walking a few laps around the house to get the blood flowing. If after doing an exercise to relieve pain such as the tennis ball exercise, or are unsure that your execution is correct, be sure to contact a podiatrist for further instruction.
Diabetic Foot Problems

Diabetes can lead to various foot problems due to its effects on circulation and nerve function. Peripheral neuropathy, a common complication of diabetes, causes numbness, tingling, or loss of sensation in the feet, increasing the risk of injuries going unnoticed. Poor circulation can impair wound healing, leading to infections and ulcers. To give themselves the best chance of maintaining healthy feet, individuals with diabetes should prioritize proper foot care. This includes daily inspection for any cuts, blisters, or changes in skin color or temperature, wearing well-fitted shoes and socks, and keeping blood sugar levels under control. Regular visits to a podiatrist are important for diabetic foot care. Podiatrists can perform comprehensive foot exams, provide guidance on preventive measures, such as proper nail trimming and callus removal, and offer treatment for foot conditions, including wound care, infection management, and custom-made orthotic devices to alleviate pressure points. If you have diabetes, it is strongly suggested that you are under a podiatrist’s care to prevent and manage diabetic foot problems.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Andrew Katz, DPM from Allcare Foothealth Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Palmdale, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes affects millions of people every year. Blood vessels located all over the body are damaged due to diabetes—even the blood vessels of the feet. Neuropathy, or nerve damage, can result from slower blood flow in the legs and feet. In diabetic patients, neuropathy is very important to monitor, as diabetics are at risk for developing ulcers.
Always washing and thoroughly drying the feet are pertinent parts of diabetic foot care. There should be a focus on cleaning between the toes. Even if no pain is felt, the entire foot should be examined for redness and sores. Neuropathy can often mask the pain of sores and ulcers and can cause these conditions to be overlooked. Use a mirror to examine the underside of your feet if needed. It is recommended that diabetics wear well-fitting socks.
Patients with diabetes should have their doctor monitor their blood levels because blood sugar levels play a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised. It is very important to keep your blood sugar levels in the normal range, which can be determined by your physician. There are medications that may be prescribed to help with any neuropathy experienced by the diabetic patient. It is also advisable to visit a podiatrist if one is experiencing any conditions involving the feet, such as ingrown toenails, which in more severe cases can cause infection.
Diabetic feet must be inspected daily. Diabetic foot care at home is possible if a patient is provided with instructions from their podiatrist. Patients can relieve dry heels with creams or ointments. Suspected wounds should warrant an immediate call to the podiatrist. Gangrene is a serious problem for diabetics and can lead to sepsis and amputation in its worst cases. Early treatment and daily inspection of diabetic feet are keys to staying healthy.
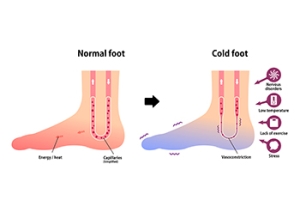
Causes of Chronic Cold Feet
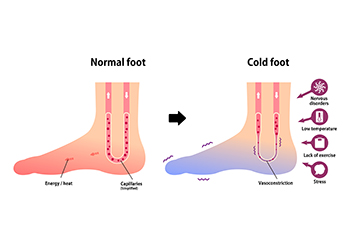
Finding the cause of cold feet is important for both comfort and overall health. While environmental factors may contribute to occasional coldness in the extremities, persistent cold feet could indicate underlying issues. One major issue is poor circulation, often linked to heart conditions, sedentary lifestyles, or smoking. Iron-deficiency anemia is another common cause of cold feet, necessitating dietary changes and supplementation. Diabetes, particularly types 1 and 2, can lead to cold feet from nerve damage, underscoring the importance of blood sugar management. Further, hypothyroidism, peripheral vascular disease, Raynaud’s phenomenon, and arteriosclerosis can all contribute to cold feet. If you are experiencing recurrent cold feet or associated symptoms, like numbness or tingling, it's suggested that you make an appointment with a podiatrist for an evaluation, diagnosis, and treatment options.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Andrew Katz, DPM of Allcare Foothealth Center. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our office located in Palmdale, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.